As healthcare leaders look ahead to 2026, one theme is emerging with growing clarity: nutrition is no longer viewed solely as lifestyle advice. According to recent coverage in U.S. News & World Report examining top health and nutrition trends for 2026, Food as Medicine is gaining traction as a practical, evidence-informed approach to prevention and chronic disease management.
While advances in pharmaceuticals and digital health tools continue to shape care delivery, experts increasingly point to diet quality and access to nutritious food as foundational drivers of long-term health outcomes.
Why Food as Medicine Is Rising Now
The growing attention to Food as Medicine reflects several converging realities:
- Chronic diseases such as diabetes, heart disease, and hypertension remain leading drivers of healthcare costs and utilization.
- Diet quality plays a significant role in both the development and management of these conditions.
- Traditional nutrition counseling often fails to account for barriers such as affordability, access, and the ability to consistently obtain healthy foods.
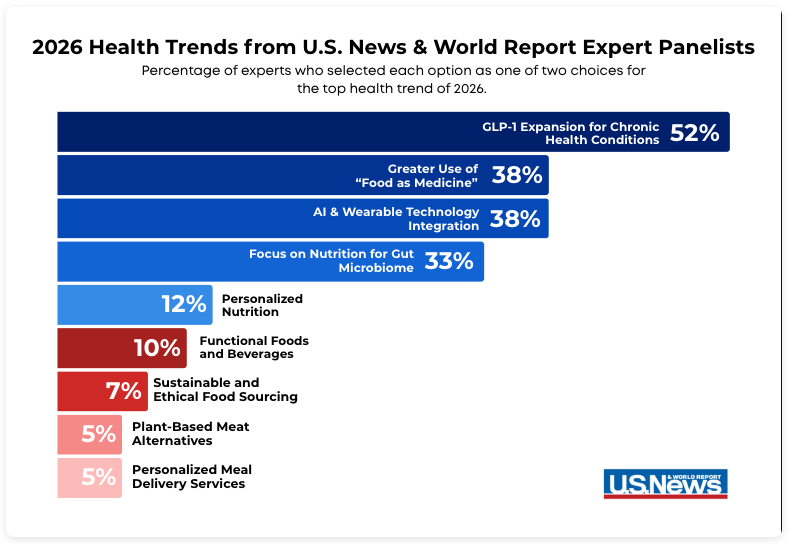
In the U.S. News & World Report trends analysis, health experts identified Food as Medicine as one of the most influential nutrition-related themes heading into 2026—placing it alongside emerging technologies and personalized health tools in terms of impact. 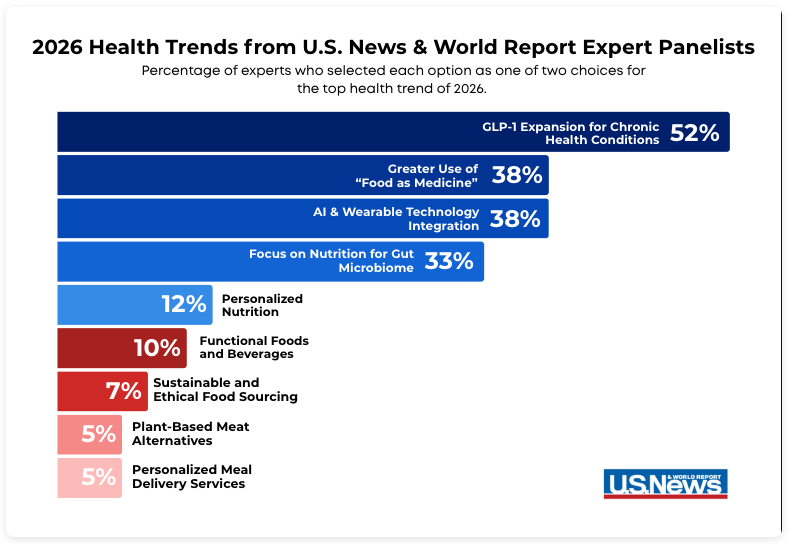
From Dietary Advice to Integrated Care
The Food as Medicine movement represents a shift from telling patients what they should eat to supporting how they can eat in practice.
Across health systems and community-based programs, this shift increasingly includes:
- Screening patients for food and nutrition-related barriers
- Aligning nutrition support with clinical goals for diet-sensitive conditions
- Connecting patients to reliable access to fruits, vegetables, and other nutrient-dense foods
- Coordinating nutrition support with broader care plans and follow-up
This evolution reflects a broader recognition that prevention and disease management are more effective when nutrition is treated as a core component of care delivery rather than a standalone recommendation.
Aligning With Broader Nutrition Trends
The same expert discussions cited by U.S. News & World Report continue to reinforce dietary patterns rich in whole foods—such as fruits, vegetables, whole grains, legumes, and healthy fats—as consistent contributors to long-term health.
These patterns are not new, but their growing integration into clinical and population health strategies signals an important change: nutrition is being operationalized, not just recommended.
How Project FoodBox Brings Food as Medicine Into Practice
Project FoodBox has long worked at the intersection of nutrition access and healthcare delivery. Our programs are designed to help clinicians extend care beyond the exam room by connecting eligible patients with medically aligned food resources that support their treatment plans.
Through partnerships with healthcare providers and health plans, Project FoodBox supports Food as Medicine by:
- Delivering nutritious food directly to patients managing diet-sensitive conditions
- Aligning food offerings with clinical guidance and dietary needs
- Reducing access barriers that often limit the effectiveness of nutrition counseling
- Supporting care teams with referral pathways and program coordination
By embedding food access into the care experience, Project FoodBox helps translate nutrition guidance into consistent, real-world support.
Looking Ahead to 2026 and Beyond
The growing prominence of Food as Medicine in 2026 health trend forecasts reflects a broader shift toward prevention, equity, and outcomes-based care. As healthcare systems continue to seek sustainable ways to improve population health, nutrition access is increasingly recognized as both a clinical and economic consideration.
For Project FoodBox, this trend reinforces our core mission: ensuring that nutritious food is accessible, aligned with care, and positioned as a meaningful contributor to long-term health.